Keratoconus is a degenerative disease of the cornea that can be highly disabling over the years. It affects one in 500 people, more or less severely, with a higher incidence among young people, teenagers and children.
If not promptly diagnosed or not treated properly, it can lead to corneal transplantation. It is a highly debilitating disease as it affects patients with high life expectancy and with good vision.
The modern diagnostic and therapeutic strategies developed in Italy help to diagnose the disease early and to block the evolution and the resulting future damage to vision, as well as to the quality of life of the subject.
Dr. Bellone what are the symptoms of this disease?
Symptoms can be diverse: usually it is manifested by a gradual loss of vision, astigmatism and myopia, night halo effects and eye rubbing. The cause of the disease is still unclear, but there seems to be a genetic predisposition (shown in 10-15% of cases). Within the same family this disease affects the various members in a “patchy” way, it is usually bilateral (85%) and severity can vary from person to person.
Dr. Bellone, why should this disease be diagnosed early?
Keratoconus more frequently affects young subjects, adolescents or children. By affecting people at a young age and therefore with a long life span the social impact of this disease is significant.
Keratoconus greatly reduces the quality of life and has a terrible psychological effect on the patient. If I told you that you are suffering from a disease that can not be cured, but can only get worse in time, how would you feel?
We must also clarify the term “disabling”: I think for a young patient to begin a long series of visits, of glasses, of contact lenses that then are not a true therapy, a pilgrimage to various specialists that can go on for years until a corneal transplant, is debilitating because it conditions the quality of life for a number of and for too many years.
And so what can we actually do?
First, focus on early detection. Being able to diagnose the start of keratoconus in the eye of a very young patient, maybe 12 years old, gives us a significant advantage over the disease and we can prevent some damage from occurring, rather than settling for not having it progress after it has occurred.
Is keratoconus difficult to diagnose? And is it more difficult with young subjects?
The advantage is that the diagnosis can be performed in a common ophthalmology clinic equipped with a corneal topographer. The most important thing is that the ophthalmologist is trained to interpret the images correctly, especially during the first signs of the disease. As with all early diagnosis efficient instrumentation and trained operators can make a big difference.
That’s why it is essential that patients gain access to specialized centers for the diagnosis and treatment of keratoconus in order to avoid misinterpretation and incorrect diagnostic treatment advice.
When diagnosed with keratoconus what is the best treatment?
I would not say best therapy, but a set of therapies that used properly can give us the best possible outcome for the framework of the individual patient. We must make good use of the weapons we have available.
Iontophoretic transepithelial corneal cross-linking is definitely one of the best weapons we have available to halt keratoconus.
Is cross-linking treatment painful?
No, it is a painless therapy and treatment times have been significantly shortened thanks to the perfecting of a successful method already widely in use.
It involves the absorption of the medicine, riboflavin or vitamin B2, inside of the ocular tissues by means of electric current at low voltage for 5 minutes.
The use of electric current, for the first time in a medical intervention, allows to obtain very high concentrations of the drug within the cornea.
Iontophoresis allows the medicine to be absorbed by the tissues in an active manner, that is, following the flow of current which carries it like train wagons carry cargo. The electric current makes it more effective: the absorption of the drug becomes much quicker and effective and time is greatly reduced, it only takes 5 minutes.
Following absorption there is a phase of irradiation of the cornea with ultraviolet UV rays for 9 minutes.
The combination of riboflavin and ultraviolet rays (both natural and available in nature) creates a chain of reactions within the cornea which lead to the formation of new corneal collagen which is healthy and not degenerated like the cornea affected by keratoconus.
Cross-linking treatment serves to create a new corneal connective tissue matrix that is more robust and functional than that of the diseased cornea.
It is a procedure free of contraindications, repeatable, performed in an ophthalmology clinic. The final result is really optimal, so much so that it can also be used with children.
Are there are other treatment options besides cross-linking and iontophoresis?
Cross-linking is only one of the cards that the ophthalmologist has available. Its function is to stop the progression of the disease, but it only acts minimally on visual defects: if a patient has become myopic and astigmatic due to keratoconus glasses cannot be eliminated following cross-linking.
So is it possible to eliminate glasses in some cases?
Over the past 20 years we have developed a surgical technique that allows for the reversal of the keratoconus to an earlier stage and thus to improve vision defects up to eliminating glasses in the most favorable cases.
The technique of implantation of Ferrara intrastromal corneal rings is ambulatory with surface anesthesia using drops. The patient goes home immediately after the surgery and already the next day can start a completely normal life.
The insertion of the rings can be performed with the help of a femtosecond laser, which is a laser capable of cutting transparent tissue with a blade of light guided by a software that can create any design in the corneal tissue.
Of course the insertion of intrastromal corneal rings must be followed by cross-linking treatment. The two techniques are mutually supportive and give optimal results when performed by highly specialized personnel.
The latest addition is the 340 ° ring essential for nipple-type keratoconus, of which I have carried out the first implant in Italy. It is a ring that is almost complete except for 20 ° which serves to be able to insert it into the corneal tunnel created beforehand with the femtosecond laser.
There are also patients who have high degrees of myopia or astigmatism. Are there no options for them at the present time?
A very interesting technique has been developed that is reserved precisely for the cases of keratoconus that are accompanied by high myopia and astigmatism and have been stable for a long time. In these cases ICL phakic lenses are implanted which are special intraocular lenses that do not need to be removed and can effectively carry out their function for a lifetime.
Keratoconus (KC) is a progressive, non-inflammatory degenerative corneal disease that can affect one or both eyes. It is hereditary in nature, typically affecting young people in the prime of their active years. It has an incidence rate of one in 500.
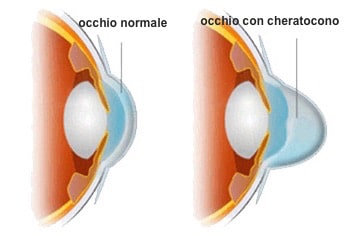
The cornea is a mass of transparent tissue that forms the front of the eye; through it we can see the iris and the pupil.
Keratoconus can lead to impaired vision and even serious damage if the disease is allowed to progress to a stage of dilation and thinning of the cornea which loses its normal spherical shape becomes cone-shaped.
To date, the causes of keratoconus are still unknown. Several researchers admit a genetic predisposition because it is observed that about 15% of those affected by keratoconus have at least one member of the family with the same disease.Some studies have focused on the imbalance of enzyme activity within the cornea, which would be more vulnerable to oxidative damage exerted by free radicals. This vulnerability would lead to a weakness in the corneal tissue resulting in thinning and reduced biomechanical resistance.Also, microtraumas caused by contact lenses and eye rubbing are indicated among the contributing factors.
Keratoconus occurs in adolescence at around 14 years of age, although the onset in childhood is not uncommon. Usually, it initially affects only one eye and after a few years it spreads to the other. Forms of keratoconus that affect only one eye are very rare.
The evolution is quite variable and unpredictable, it can spontaneously slow down, but it never stops entirely. Unfortunately, it is not considered a rare disease as we have one new case per 500 persons per year when considering topographic forms of the disease, with a slight preponderance of male subjects.
This case report was published in the journal “Cornea” on June 24, 2011.
It is well known that pregnancy produces changes in hormone levels. Sometimes these hormonal changes can affect the eyes and also patients with keratoconus.
Turkish eye specialists have identified four cases of pregnant women with keratoconus who showed signs of change in visual acuity and corneal curvature.
These women had no other diseases or risk factors for keratoconus so the researchers concluded that “the hormonal changes during the pregnancy period may adversely affect corneal biomechanics and pregnancy could be a previously unrecognized risk factor for the progression of keratoconus.
To the best of our knowledge, at present this is the first study that shows a progression of keratoconus induced by pregnancy in patients in the absence of other correlated disease.”